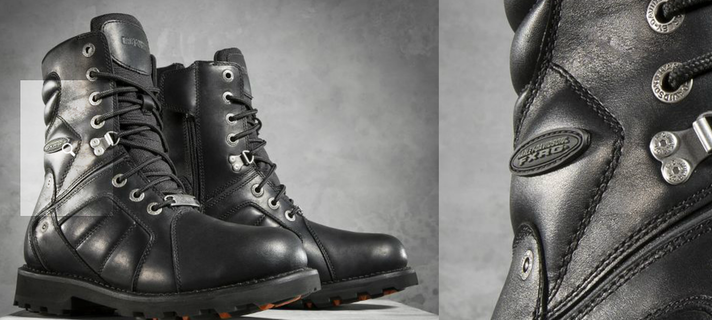
 Riding on a Hog, 10 hours a day on the laid back, truck worn highways of America can leave your feet wishing they had stayed home. There's not a method of transportation more encouraging for the soul than motorcycling. But the vibrations caused by the thumping heart of your 600lb machine can vibrate your body into submission and leave the soles of your feet feeling anything but courageous. Try traipsing around a truck stop or stepping off your bike on an a scenic overlook after a long ride; your butt is raw, your legs are noodles, and your feet? Well, there are several sensations you might experience. The three main ones are Blisters, Numbness, and Arch Pain. When you get all three, it's called "Boot Burn". Blisters: Riding boots with poor cushioning or flat or misshapen insoles can transfer vibrational forces to the foot causing friction. The soft skin of the foot is no match for leather and glues and the seams rubbing over toes and arches can create skin breakdown which ultimately causes wounds. Numbness/Tingling: Riding boots with tight toe-boxes, tight laces, or narrow and shallow heels can restrict blood flow and cause the foot to lose sensation. Attempting to walk with insensate feet can affect where and how you place your feet and bring about an unstable gait. A loss of proprioception may occur. In other words, if you cant feel your feet, you'll have a hard time knowing where your feet are underneath you, increasing the risk of falls. Arch Pain: Riding boots with inadequate mid-foot support can stress the plantar fascia (a broad, flat ligament on the bottom of your feet) beyond it's normal range and small micro-tears can develop causing pain. The symptoms of boot burn and more were topics of discussion at Grove's Harley Davidson in Winchester, Va during the Art of the Motorcycle event this October. Duane(COO) and Barbara(Owner) invited me to come talk to the bikers and staff about improving their foot health and how orthotics can maximize the fit and feel of their line of Harley Davidson riding boots. As the morning began and riders started to stream in, we discussed the topics of diabetes, in-grown toenails, shoe inspections, and how increased stress and poor foot alignment over time can cause over-use injuries such as posterior tibialis tendonitis, achillies tendonitis, and plantar fasciitis. I performed several scans and saw a multitude of feet. Education reigned supreme this day and everyone came away with a new understanding of their feet. I look forward to returning often to bring comfort and performance to the boots of riders at Grove's Harley Davidson. So what to do about Boot Burn? One answer is a combination of Dealer Exclusive Harley Davidson riding boots like the all new HD Vance FXRG and a pair of custom Graceyfeet Orthotics. The Vance is a newly released, high-performance motorcycle boot for riders who place heavy demands on their gear. Waterproof, with a tall vamp and roomy toebox, the Vance sports high-end riveting, double-sewn seams, and a goodyear welt. Entry is easy and quick with a full-length medial zipper. But the boot lacks a sock-liner that performs to the standard that Harley boot leathers have come to be known by. Included in the boot is a consumer-grade, inexpensive, molded gel insole. This insole is inadequate to make walking and riding comfortable. Removing this poor feature and replacing it with a Graceyfeet, full-length, medical-grade orthotic solved every issue instantly. I rank this boot in the highest category for comfort and performance so long as a custom insole is utilized. It really is the perfect boot for all your riding needs. Graceyfeet Custom insoles are CAD/CAM designed to address each of the negative conditions of boot burn and can be made medically appropriate for every rider's needs. Graceyfeet is proud to educate Harley riders on proper care of the foot and ankle and how the qualities of a riding boot can affect the riders' overall riding experience. Come find me at Harley Davidson and I'll not only give you professional, biomechanical insights, but huge discounts on custom orthotics exclusive to Harley Davidson Motor Company to help you Live Free and Stride. Thank you to Barbara, Duane, Jeff, Raymond, Chris, Kim, Chuck, and all the patrons and staff at Grove's Harley Davidson of Winchester. See you again soon!
1 Comment
In this episode of Living Healthy, I discuss who I am, some easy to understand concepts of the foot and ankle, and the Graceyfeet product line. What I did not have time for was to convey the understanding that the bridge between foot comfort and wellbeing extends beyond the physical and scientific theories described by scientists in peer-review journals. That my orthotics reach beyond the objective alignment of the joints and reduced foot pressures to touch the very soul of the wearer at the heart of their anxiety. Graceyfeet orthoses encourage a process of learning to recognize and observe (mind) the reactions and habitual patterns of a foot fall (body) and the resulting effort (breath) you extend during your functional day. Graceyfeet orthoses strive to align the bones, joints, and muscles, thereby enhancing strength and flexibility, balanced muscle action, and stamina and endurance. They are tuned to your perceived comfort and the more you wear them, the sooner you will discover the right balance between ease and effort in standing and walking. You'll be lengthening and contracting your muscles, aligning and gliding your joints, and quieting and soothing your nervous system as your Sole Commander orthoses guide your center of progression on its most correct path. They seek to bring about a mindfulness of motion.
Huge Hug and Thank You to Jay Greenstein and Barton Bishop for inviting me to come on and share my passion for making feet feel good. You may contact me by email ( graceyfeet@aol.com ) or at any one of the 7 Sport and Spine Rehab locations throughout the DC/MD/VA area. God is good, Peace be with you, and Namaste' Chris http://www.prweb.com/releases/2013/11/prweb11323572.htm Chris  Volleyball, Basketball, Football, Track, Cheerleading...there are many sports that require an athlete to leap. Sometimes pain can occur in the ball of the big toe reducing the person's ability to perform to their desired capacity. Lost time off the court can hurt the team and in some cases, ruin a career. The scientific discussion below illustrates one of the problems that can occur in the foot. Plainly said, toe pain can be a product of poor alignment, stress, and overuse. A quality orthoses can correct the alignment, reduce stress, and restore pain-free balance. Hallux rigidus typically presents as an isolated arthritis in the adult without a systemic arthritic condition. This suggests the degenerative process is caused by some local pathologic alteration in the first MTPJ. The athlete with hallux rigidus usually complains of pain at this joint. He or she will often complain of stiffness and decreased motion with certain activities. Usually extension of this joint is limited, which reduces an athlete's ability to push off and causes them pain. Secondary joint degeneration may occur after a recognized traumatic event. Other theories suggest hallux rigidus is caused by extra strain on the first MTPJ in a pronated foot or by an elevated first metatarsal, resulting in a limitation of hallux dorsiflexion. In any case, the condition tends to be progressive. Normal range of dorsiflexion motion of the first MPJ should be 65 to 75 degrees in order to allow for a normal gait. Near the end of the propulsive phase of gait, the leg has a 45-degree position to the floor and the ankle is in about 20 degrees of plantarflexion to the leg. This position requires the hallux to be able to dorsiflex 65 degrees. Anything less requires accommodation or adaptation from the surrounding joints. This compensation can come from gait changes, such as subtalar joint supination and walking on the outside of the foot, subtalar joint pronation with foot abduction, etc. The treatment of hallux rigidus is aimed at reducing the local inflammatory process at the first MTPJ and decreasing the dorsiflexion forces that lead to painful dorsal impingement. The initial thrust should be to decrease the acute inflammatory reaction by emphasizing rest, NSAIDs and ice. Graceyfeet Sole Commander and Sole Supporter orthoses seek to relieve the painful forces by repositioning the 1st metatarsal head and spreading vertical forces towards the lateral foot. This allows for use of the client's full available ROM at the 1st MTP during forefoot loading in late stance phase of gait. Decreased pain and increased function are the results! Contact Chris at Graceyfeet@aol.com and chat with him about additional ways you can improve performance and prevent injury in your team. J Orthop Sports Phys Ther. 1999 Dec;29(12):727-35. Nonoperative and operative intervention for hallux rigidus.Nawoczenski DA. J Orthop Sports Phys Ther. 2009 Oct;39(10):733-42. doi: 10.2519/jospt.2009.3003. Structural factors associated with hallux limitus/rigidus: a systematic review of case control studies.Zammit GV, Menz HB, Munteanu SE.  As beginner golfers are acutely aware, the body motions of golf can feel and look as awkward as a seagull on a seesaw. As the new duffer progresses, it is traditional to model elements of his or her swing after the professional players they follow; A bit of Ben Hogan head-dip on the take-away, Tiger Woods’ torso turn at the top of the backswing, or Vijay Singh’s narrow attack on the downswing. So whose feet do you follow? Are they live or still? Sam Snead or Bobby Tway? Scientific golf studies have identified several key elements in the golf swing that can differentiate the skill level of golfers. The sequential pattern of swing involves movement of different segments of the body and interactions with the club at particular moments in time and through several necessary ranges. These motions require skill and timing in order to produce an optimum shot. But what's going on at the foot?? I find it to be one of the most simple yet confusing parts of the golf swing. First, the swing... We know all about the body in swing...Bunn (1972) described that the proximal body segments theoretically should reach their peak speed first, followed by more distal segments to execute an efficient and powerful motion during the golf swing. Thus, a proper golf swing should be initiated by motion of the pelvis, followed by that of the upper trunk, upper extremity, and then the golf club, in order to transfer momentum from proximal parts of the body to the distal segments. However, The feet play the role of dynamic stability...Kawashima Kazuaki investigated the intensity of force on the big toes of both feet during the golf swing. He looked at four right-handed golfers; a male tournament professional-golfer, a male amateur golfer (HDCP 16), a female tournament professional-golfer, and a female amateur golfer (HDCP 20). There were obvious differences among four golfers in the swing movement, comparing the intensity of force of the right and left big toes. The findings were as follows: The Male and female golfers demonstrated a gradual increase in force on his both big toes with the value 14 Ns and 11 Ns, respectively. Conversely, the male amateur golfer exhibited high force (11 Ns) on the left big toe only. Both the male and the female pro-golfer and the male amateur showed higher force during the back swing (A-T) phase, compared with other phases, e.g. downswing (T-I) and follow-through (I-F). The female amateur golfer showed higher force at I-F phase. It may be considered that during back swing, the more skillful golfer puts force on the big toes of both feet. Results of this study indicated that toe force at A-T phase is an important factor that is required, in order to hit a ball correctly and with power. Here's Rocco Mediate demonstrating the subject barefoot.... http://www.youtube.com/watch?v=riwWLct4DrA "Where my weight is going...towards my toes, not my heel" He says. So based on Kazuakis' study, Rocco appears to be a great person to emulate for proper lower extremity position and foot force during the back swing. However, the down swing and finish position of the foot belongs to Tiger. In 2012, I had the opportunity to collaborate with PGA Pro Bernie Najar of Caves Valley GC in Baltimore, Maryland. His state of the art biomechanics lab features cameras, screens, and specialized computer programs that can capture a player's every movement. Together, we analyzed Tiger Woods' swing to discover a fix for a painful neuroma. It appeared on observation that Tiger internally rotated his hip during follow-through at a specific moment, allowing his heel to arc and rise into a position that pointed his toe perpendicular to his left foot. His left foot, was supinated at terminal swing to the point his great toe was off the ground and he was bearing weight on the lateral boarder of his foot. A morphologically distant indicator of adequate transverse pelvic rotation. The adoption of this style of lower extremity positioning resulted in a reduction of pain in the right foot during the swing. Wearing a custom molded Graceyfeet Sole Commander orthotic and a premium Graceyfeet Cush insole in his shoe, Bernie had a maximum shot spread over 15 shots using a 7 iron that was no more then 5 yards in 360deg. Increased distance was noted after the technique change as well. Success! Barton Bishop of Sport and Spine Rehab in Rockville, MD marvels at the many ways foot orthotics can help reduce pain on the golf course. One way, as Bernie and I found out, was through emulating Tiger Woods and his swing mechanics. You go Bernie Najar!  Cheerleading is often overlooked as an injurious sport and scant studies have focused on the mechanisms and incidences of injuries. But the reality is that cheerleading has evolved over the past century-and-a-half from a pep-group chanting in the bleachers to a competitive combination of high-impact dance and extreme-skill performance sport: filled with high-flying stunts and dangerous skills. Cheerleading has quickly become one of the most necessarily accurate professional sports due to the advancement of trick stunts and the subsequent improvements in training practices. In order to pull off those high-flying moves, athletes must train daily at intensities formerly reserved for the team sports they cheer for. Thus, they are subject to common over-training injuries which include ligamentous sprains, muscular strains, fractures, and contusions. Dr. Jay Greenstein, CEO of Sport and Spine Companies in the Washington, DC area and a leader in the chiropractic industry at the national level offers his insight: “Cheerleaders suffer lots of lower extremity injuries. A 2012 study published in the Journal of Trauma and Acute Care Surgery revealed that lower extremities injuries made up approximately 30% of all cheerleading injuries seen in the emergency room over a 5 year period. A study published in the American Journal of Emergency Medicine reported that an even higher rate of lower extremity sprains and strains at 42% of total injuries occurring. Athletes should be aware that muscle compensations due to injuries of this nature create postural imbalances that can go unnoticed resulting in alignment issues that have a deeper affect on a person's performance and safety. An early evaluation for orthotic need can assist in reducing the risk of posterior tibial tendon, achilles tendon, and peroneal (fibularis) sprains and strains. In 2011, Franklyn-Miller, A,et.al. found the use of customized foot orthoses during training for those assessed as being at-risk resulted in a 20% reduction in lower limb overuse injury rate. Stabilizing the body through guided and controlled rehabilitation, skeletal manipulation, and orthotic use can keep the body aligned, improve sensorimotor control, and maintain better balance. Dr. Greenstein continues:"While functional elements of muscle imbalances, prior injury, and thus poor sensorimotor function are key variables of this epidemic, we also realize that there are anatomic variables that must be addressed. In a study published in the Clinical Journal of Sports Medicine, the application of a custom foot orthoses “have an immediate effect on (lower extremity) dynamics.” So, in thinking about prevention first, having a pre-emptive evaluation to determine the need for a custom orthoses to improve lower extremity dynamics and function, and reduce the risk of injury, is a worthwhile endeavor.” A cheerleading-specific lower extremity evaluation will include objective measures of range of motion, strength, spinal alignment, pelvic obliquity, leg length discrepancy, knee alignment, hindfoot alignment, plantar fascia patentcy, sub-talar joint axis, navicular drop, flexor hallucis congruency, heel-ball ratio, and forefoot to hindfoot alignment during static and weightbearing sport maneuvers. In fact, these elements are necessary to fabricate the most appropriate device for any person seeking to improve their performance through balance and injury prevention. Notes on Cheerleading injury incidence and prevention In 2002, the Journal of Pediatrics published an epidemiological review of cheerleading injuries in children from 1990-2002. The authors found the body parts injured were lower extremity (37.2%), upper extremity (26.4%), head/neck (18.8%), trunk (16.8%), and other (0.8%). Injury diagnoses were strains/sprains (52.4%), soft tissue injuries (18.4%), fractures/dislocations (16.4%), lacerations/avulsions (3.8%), concussions/closed head injuries (3.5%), and other (5.5%). Children in the 12- to 18-year age group were more likely to sustain strains or sprains to the lower extremity than 5- to 11-year-olds (P < .01; RR: 1.62; 95% CI: 1.50–1.88). Since this land-mark paper was published, catastrophic injuries in cheerleading has continued to rise. The latest information (Oct 2012) shows the number of catastrophic injuries related to cheerleading has increased from 1.5 annually from 1982 to 1992 to 4.8 per year from 2003 to 2009 according to the American Academy of Pediatrics. Catastrophic injuries include closed-head injury, skull fractures and cervical spine injuries resulting in permanent brain injury, paralysis or death. New recommendations in the guidelines of injury prevention in cheerleading have just been released and include:
Thank you to Dr. Jay Greenstein for his contribution to this article. http://www.ssrehab.com/ Council On Sports Medicine and Fitness. Pediatrics. 2012;doi:10.1542/peds.2012-2480. J Physiother. 2011;57(3):193. Foot orthoses can reduce lower limb overuse injury rate.Landorf KB. SourceLa Trobe University, Australia. PEDIATRICS Vol. 117 No. 1 January 1, 2006 pp. 122 -129 (doi: 10.1542/peds.2005-1139) American Academy of PediatricsPolicy Statement: Cheerleading Injuries: Epidemiology and Recommendations for Prevention
 Every shoe company has an idea of how thin a sole should be or what the heel to forefoot relationship should be and their guidelines are not well defined. What exactly is a "Minimalist" shoe? The parameters and features of a minimalist shoe vary greatly and even their marketed usages may differ widely, but the shoe industry continues to pursue persons willing to cough up a little extra money for a little less material under-foot. As in all life, the past repeats it's self often enough that we can find the answers in historical terminology. Shoes were once exclusively named for the type of sport they were meant for and later for the properties of their construction. "Trainers", "Field Cleats", "Tennies", and "Racing flats" were all an athlete needed to ask for 40-50 years ago when the mass marketing of shoes was in it's infancy. There were no large heeled, anti-pronation, asymmetric, multi-durometer, extruded soles on the market because designs were yet to be drawn, the machines had yet to be invented, the sports had yet to be integrated into society, and marketeers had yet to exploit the idea that running barefoot was somehow healthier for you. Later, as running took hold as a common sport and past-time, helpful terms such as "Half-Last", "Board-Last", "Straight or Curved Last" came into vogue as a means of better educating the consumer on selecting proper footwear. The term "Minimalist Running Shoe" is primarily used to group together styles of shoes with attributes that yield a walking or running experience similar to being barefoot without allowing the plantar surface of the foot to make direct contact with the ground. Minimalist running shoes (MRS) are lightweight, low to the ground, and flexible. They provide very little cushioning for the heel and forefoot. Additionally, compared to traditional running shoes, there is minimal slope from the heel to the forefoot in the MRS. This reduction in cushioning and decreased heel-to-toe drop forces the runner to land with a more anterior foot strike when running. While there are anecdotal stories of these MRS reducing injury and improving performance, there are still no conclusive research studies that confirm these claims. What does seem clear is that switching from a traditional running shoe to a MRS requires a proper transition period to avoid potential overuse injuries. There is no one right way to make the transition to MRS, but most programs require a period of 8-12 weeks. Running with MRS encourages a forefoot or midfoot strike when running. This type of foot strike means that rather than landing on your heel, you will land on the toes or mid part of the foot. This landing may lead to a reduced initial impact force on landing and relies on strong foot and leg muscles. A good transition program will focus on learning how to land on your forefoot or midfoot and will include strength exercises specifically for the foot and leg. Another important aspect of the transition is that you start with very short distances using the MRS – and build gradually over several weeks. This might be more easily said than done. While some studies show a reduction in vertical forces experienced in the joints, others suggest barefoot running requires more strength and has a greater metabolic cost on the body compared to shod running. Even the world's elite runners heel-strike; Meb Keflezighi and Usain Bolt both heel-strike as a primary method of running. Ankle and Tibial bone injuries are associated with heel-striking over use injuries while metatarsal fractures, posterior tibialis tears, plantar fasciitis and musculotendinous strains are associated with mid-foot strikers. Whether you are for or against near-barefoot running, one thing is very clear: A persons body will tend to stand, sway, walk, and run in the most metabolically efficient way to bring about the most amount of comfort in any situation they encounter. Specialized shoes and conscious changes in running styles has the effect of increasing energy consumption which, in turn, causes earlier fatigue. There is no one way to run! In the absence of pathology, your natural gait and movement patterns are the ideal method of performance for you! Graceyfeet insoles allow you to move within your preferred path of progression but lower the detrimental ground reaction forces that travel through the plantar surface of your foot an cause you injury and pain up the chain. They are the perfect compliment to any minimalist shoe. Lieberman DE, Venkadesan M, Werbel Wa, et al. Foot strike patterns and collision forces in habitually barefoot versus shod runners. Nature 2010;463(7280):531-535.: http://www.nature.com/nature/journal/v463/n7280/full/nature08723.html Miller RH, Umberger BR, Hamill J, Caldwell GE. Evaluation of the minimum energy hypothesis and other potential optimality criteria for human running. Proc Biol Sci 2012;219(1733):1498-1505. : http://lowerextremityreview.com/issues/may/biomechanist-challenges-idea-that-forefoot-strike-pattern-reduces-runners-injury-rate FOOT CONTACT PATTERNS AND JOINT DEMANDS IN NOVICE BAREFOOT RUNNERS BEFORE AND AFTER EXERTION Hashish R, Samarawickrame S, Powers C, Salem G CSM 2012 Sports Physical Therapy Section Abstracts: Poster Presentations SPO1100-SPO1125J Orthop Sports Phys Ther 2012;42(1):A114-A124  The effect of muscle fatigue on in vivo tibial strains Journal of Biomechanics Accepted 12 March 2006 published online 9 May 2006 Stress fracture is a common musculoskeletal problem affecting athletes and soldiers. Repetitive high bone strains and strain rates are considered to be its etiology. The strain level necessary to cause fatigue failure of bone ex vivo is higher than the strains recorded in humans during vigorous physical activity. We hypothesized that during fatiguing exercises, bone strains may increase and reach levels exceeding those measured in the non-fatigued state. To test this hypothesis, we measured in vivo tibial strains, the maximum gastrocnemius isokinetic torque and ground reaction forces in four subjects before and after two fatiguing levels of exercise: a 2km run and a 30km desert march. Strains were measured using strain-gauged staples inserted percutaneously in the medial aspect of their mid-tibial diaphysis. There was a decrease in the peak gastrocnemius isokinetic torque of all four subjects’ post-march as compared to pre-run (p=0.0001), indicating the presence of gastrocnemius muscle fatigue. Tension strains increased 26% post-run (p=0.002, 95 % confidence interval (CI) and 29% post-march (p=0.0002, 95% CI) as compared to the pre-run phase. Tension strain rates increased 13% post-run (p=0.001, 95% CI) and 11% post-march (p=0.009, 95% CI) and the compression strain rates increased 9% post-run (p=0.0004, 95% CI) and 17% post-march (p=0.0001, 95% CI). The fatigue state increases bone strains well above those recorded in rested individuals and may be a major factor in the stress fracture etiology. Effects of Fatigue on Running Mechanics Associated with Tibial Stress Fracture Risk. Clansey AC, Hanlon M, Wallace ES, Lake MJ. Med Sci Sports Exerc. 2012 Apr 19. PURPOSE: The purpose of this study was to investigate the acute effects of progressive fatigue on the running mechanics parameters previously associated with tibial stress fracture (TSF) risk. METHODS: Twenty one male trained distance runners performed three sets (Pre, Mid & Post) of six overground running trials at 4.5 m·s (± 5%). Kinematic and kinetic data were collected during each trial using a twelve-camera motion capture system, force platform, and head and leg accelerometers. Between tests, each runner ran on a treadmill for 20 minutes at their corresponding lactate threshold (LT) speed. Perceived exertion levels (RPE) were recorded at the 3 and last minute of each treadmill run. RESULTS: RPE scores increased from 11.8 (± 1.3) to 14.4 (± 1.5) at the end of the first LT run and then further to 17.4 (± 1.6) by the end of the second LT run. Peak rear foot eversion, peak axial head acceleration, peak free moment and vertical loading rates were shown to increase (p < 0.05) with moderate-large effect sizes during the progression from Pre to Post tests, although vertical impact peak and peak axial tibial acceleration were not significantly affected by the high intensity running bouts. CONCLUSION: Previously identified risk factors for impact-related injuries (such as TSF) are modified with fatigue. As fatigue is associated with a reduced tolerance for impact, these findings lend support to the importance of those measures to identify individuals at risk of injury from lower limb impact loading during running. The Influence of Muscle Fatigue on Electromyogram and Plantar Pressure Patterns as an Explanation for the Incidence of Metatarsal Stress Fractures Background: Stress fractures are common overuse injuries in runners and appear most frequently in the metatarsals. Purpose: To investigate fatigue-related changes in surface electromyographic activity patterns and plantar pressure patterns during treadmill running as potential causative factors for metatarsal stress fractures. Study Design: Prospective cohort study with repeated measurements. Methods: Thirty experienced runners volunteered to participate in a maximally exhaustive run above the anaerobic threshold. Surface electromyographic activity was monitored for 14 muscles, and plantar pressures were measured using an in-shoe monitoring system. Fatigue was documented with blood lactate measurements. Results: The results demonstrated an increased maximal force (5%, P < .01), peak pressure (12%, P < .001), and impulse (9%, P < .01) under the second and third metatarsal head and under the medial midfoot (force = 7%, P < .05; pressure = 6%, P < .05; impulse = 17%, P < .01) toward the end of the fatiguing run. Contact area and contact time were only slightly affected. The mean electromyographic activity was significantly reduced in the medial gastrocnemius (-9%, P < .01), lateral gastrocnemius (-12%, P < .01), and soleus (-9%, P < .001) muscles. Conclusion: The demonstrated alteration of the rollover process with an increased forefoot loading may help to explain the incidence of stress fractures of the metatarsals under fatiguing loading conditions. A concussion is a pathologic process affecting the brain induced by rapid brain movement inside the skull. It is a brain injury that has life altering effects and can manifest in a person as trouble in school, relationships, work, and play. Perception of situations, decision-making, and problem solving are all possibilities.
In 2009 alone, there were documanted 3.8 million sports related concussions in the US. 40-60 thousand in HS football alone, yet only 6% go to the ER. Symptoms include: Head Ache, nausea/vomiting, decreased balance, decreased vision, feeling "foggy" or confused, and memory problems. Observations include: Dazed look, cannot follow instructions, mood changes, memory problems such as not being able to recall the hit or not remembering plays. People with one concussion are 2-4x more likely to have another concussion. 80% of all concussions occur less than 10 days from the first. NO SAME DAY RETURN TO SPORT! Got a Concussed Player? Remove from play Monitor for worsening symptoms Discuss findings/suspicions with coaches, player, and parents Make sure they are symptom free and cleared before returning to play. Report it! When to call EMS/911: Observed increased confusion, loss of consciousness, neck/spine involvement, and or vomiting Post injury monitoring includes: 5-10 minutes of constant attention to injured player Mental Status Memory Balance Attention Speech Graduated Return To Play: Zero activity - Phys/Cognitive testing - Recovery Lt. Aerobics - Walk/swim/bike - Incr. Heart rate Sport Specific Ex's - Running, no impact - Incr. movement Non-contact Drills - Complex Drills - Incr. Coordination Full-Contact Drills - Normal Training load - Incr. Cognitive load Return to Gameplay - Gameplay - Restore Confidence Every injury is individual! Be conservative with youth! There is no simple "Return to play" test! "When in doubt, Sit them out!" Recently, it had been reported that concussions were on the rise among High Schools in Montgomery, Co. This prompted Principal Alan Goodwin to team up with Dr. Michael Singer of Brain Scope and bring together the areas' top authorities on concussions and traumatic brain injuries. The evening was designed to educate and inform the public of the most current clinical findings and issues surrounding concussions today.
Definitions of even what a concussion truly is were discussed as well as the loss of consciousness (LOC) and a good graphic was shown to differentiate the ratings. A few quotes from the Whitman Concussion Forum: “We Don’t Know”: With mandatory helmet rules only being passed in the NFL in ’78 and required in HS and college in ’80, there are no longitudinal studies to show whether so called advancements in helmet technology have had an impact on the actual number of concussions or not. We do not know the answer to most questions surrounding concussions. “You don’t need symptoms to have a concussion”: The brain can be altered at a sub-concussion level. The level of tolerance is individual for vibrations to the brain. There is no way to test for a players’ ability to withstand repetitive concussion forces. “There is no correlation between loss of consciousness and severity of concussion”: Take a look at the recent concussions among professional players. Kobe Bryant did not lose consciousness and yet he was out for weeks while many NFL players routinely return to play after only 7 Days following a concussion. “If a child has had a concussion and recovered fully, they are considered not at risk to play. But even though there are no long-term studies currently, it is accepted that multiple concussions are bad! Heading a soccerball is not a risk if done with appropriate form and technique. The whipping of the head and collisions with other players are where the risks lie. And again, we do not know about the effect of repetitive sub-concussion forces on the human brain. |
Chris Gracey MPT, Cped
Archives
October 2015
Categories
All
|
Follow Graceyfeet on Facebook and Twitter




 RSS Feed
RSS Feed
